Michigan Medicaid Nursing Facility Level of Care Determination LOCD
Table of Content
Go to Migrant Services Our migrant program works with a number of organizations to provide services for Michigan’s migrant and seasonal farmworkers. Go to Children & Families Programs for healthy children & families, including immunization, lead poisoning prevention, prenatal smoking cessation, and many others. Find and compare freestanding nursing homes and hospital-based nursing homes in your area. Use this checklist to help you pick an assisted living facility. Caregiver services — Provides a break and other help for family members who help take care of you. To apply for the MI Choice Waiver, Michigan residents should contact the waiver agency that serves their area of residence.

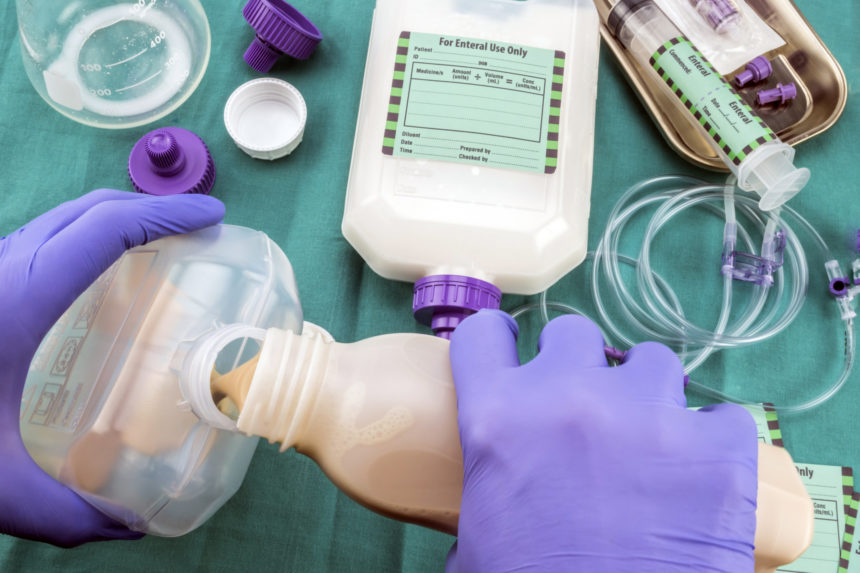
The criteria that determines NF LOC is outlined in the Michigan Medicaid Nursing Facility Level of Care Determination . If your doctor says you need full-time care from a nurse, a nursing home may be right for you. Nursing homes are the highest level of care most people will receive outside of a hospital. In additional to a high level of medical care, residents get help getting into and out of bed and with feeding, bathing and dressing and other activities.
Why Would I Need Long-term Care?
Michigan Aged Blind and Disabled Medicaid beneficiaries who can not perform all of their Activities of Daily Living and Instrumental Activities of Daily Living can receive help with these activities through the Home Help Program. In order to be eligible for this program, applicants must need hands-on assistance with at least one Activity of Daily Living. Michigan uses an Adult Services Comprehensive Assessment (MDHHS-5534) to make this determination. The need for help can be due to aging, illness or cognitive issues caused by Alzheimer’s Disease or other dementias. A downside is that they charge hourly and can be expensive, at hundreds of dollars per hour.
No individual will be required to change nursing homes resulting from this transition; however, new placements will be based upon the MCO´s contractual arrangements and the needs of the individual. MCOs must evaluate and ensure that individuals are placed in the least restrictive setting with needed community supports. People who are older and require help with basic tasks of living – bathing, dressing, personal care, housekeeping or preparing meals – are candidates for long-term care services. Long-termCare.gov estimates that as many as 70 percent of people turning 65 can expect to use some form of long-term care during their lives. During the process of determining financial eligibility, it’s important to start gathering documentation that clearly details the financial situation for the Michigan Medicaid applicant. These documents will be needed for the official Michigan Medicaid application.
The roles of the local department of social services, the MCO and the nursing home post transition
The plan´s assessments are in addition to any assessment required of the hospital, nursing home or other providers. The assessment and the medical provider´s order become the basis for determining the needs of the member. During the assessment process and the care planning process, the member is made aware of all services available through the plan. They are also made aware of services that are not included in the benefit package but are Medicaid services under the fee for service program. The MCO must implement a written care plan and assist the member in accessing the services authorized under the person centered services plan. When an individual moves to long term placement in a nursing home from a community setting or rehabilitative stay, the process must be a consumer oriented transition.

The cost of a nursing home in Texas ranges from $3,000 to $4,000 a month . If you do not have much income or other resources, Medicaid may pay for a nursing home. You can talk to a Texas Health and Human Services employee about Medicaid. You will have to live in a nursing home for 30 consecutive days before you can apply for services. One’s home is often their most valuable asset, and if counted toward Michigan’s Medicaid asset limit, it would likely cause them to be over the limit for eligibility. However, in some situations the home is not counted against the asset limit.
I. Eligibility and Enrollment
Benefits include help with Activities of Daily Living and Instrumental Activities of Daily Living . Note for Married Couples – While a single nursing home Medicaid beneficiary must give Medicaid almost all their income for nursing home care, this is not always the case for married couples in which only one spouse needs Medicaid-funded nursing home care. There are Spousal Protection Laws, which protect income and assets for the non-applicant spouse to prevent spousal impoverishment.
For instance, a service plan for a senior with early stage Parkinson’s disease dementia might indicate 20 hours of personal care assistance and homemaker services is required, as well as home modifications to continue to safely live at home. Michigan residents have to meet an asset limit and an income limit in order to be financially eligible for Aged Blind and Disabled Medicaid / Regular Medicaid. The 2022 income limit for a single applicant is $1,133 / month.
Department of Health
Besides income, your assets will be counted toward meeting eligibility requirements. Countable assets include checking and savings account balances, CDs, stocks, and bonds. Some states may also require a physician diagnosis of specific medical conditions or a statement that the Medicaid applicant requires the level of care provided in a nursing home. Specific to each state, the general or usual responsibilities of the NF are shaped by the definition of NF service in the state's Medicaid state plan, which may also specify certain types of limitations to each service. States may also devise levels of service or payment methodologies by acuity or specialization of the nursing facilities.
Medicaid pays a fixed daily rate so a nursing home Medicaid beneficiary does not have to pay any part of the cost. The principles below must be defined formally clarified between all parties in order to operationalize and promote appropriate discharge planning and care management. The MCO will make a coverage and medical necessity determination for requested services, equipment and supplies for the member taking into consideration the results of the full UAS-NY assessment and other assessments conducted by the NH.
To be eligible for Michigan Medicaid, a person has to meet certain financial requirements and functional requirements. MI Health Link HCBS Waiver beneficiaries must need a Nursing Facility of of Care. To see if this level of care is required, the state uses the Michigan Medicaid Nursing Facility Level of Care Determination. This also helps the state determine which program benefits each individual will receive.
Medicaid is separate from Medicare, which is a federal program that pays certain healthcare expenses for individuals ages 65 and older. It is estimated that between 80% and 90% of nursing homes accept Medicaid. While this percentage sounds high, these percentages are very misleading.
The most common functional consideration is one’s ability / inability to perform one’s activities of daily living (bathing, dressing, grooming, etc.). The questions may ask how often (how many times per day / how many days per week), for how long , and what type of assistance (verbal cues, assistive devices / adaptive equipment, hands on assistance, 100% dependent) a person requires. As part of the care plan development, or afterward, the MCO may review the proposed care for service coverage and medical necessity. The time to review a request for long term placement begins with the provider´s recommendation for placement and request to the MCO for transfer to a SNF. The MCO will make medical necessity determination as fast as the enrollee´s condition requires and within the timeframe mandated by the MCO contract with the State.
Comments
Post a Comment